So, you’re on a course of antibiotics and wondering if you can continue using cannabis. The short answer is: yes, cannabis can affect antibiotics, but it’s not the dramatic, sudden reaction you might be picturing.
The real issue is a subtle, behind-the-scenes competition happening in your liver. This interaction can change how your body handles the medication, which could potentially weaken its effect or ramp up the side effects.
The Straight Dope on Mixing Cannabis and Antibiotics
When you’re fighting off an infection, the last thing you want is to accidentally sabotage your treatment. Understanding how cannabis and antibiotics can interact is your first step toward making smart health choices and ensuring a smooth recovery.
It all comes down to your body’s primary processing plant: the liver.
Think of your liver as a busy factory with a specialized crew of workers. These workers are enzymes, specifically a group called the Cytochrome P450 (CYP450) system. Their job is to break down everything from your lunch to the medications you take. Here’s the catch: both cannabis compounds (like THC and CBD) and many common antibiotics need this exact same crew to get processed.
A Battle for Your Body’s Resources
When you have both cannabis and an antibiotic in your system, they start competing for the attention of those CYP450 enzymes. It’s like two urgent jobs landing on the same desk at once.
This competition can play out in a couple of ways:
- Slowing things down: Cannabis might monopolize the enzymes, forcing the antibiotic to wait its turn. This means the medication breaks down much more slowly, leading to higher-than-intended levels of the drug in your bloodstream.
- Speeding things up: In other scenarios, cannabis could kick the enzymes into overdrive, causing them to break down the antibiotic too quickly. This lowers the drug’s concentration and robs it of the time needed to work.
This is exactly why your doctor would urge caution. For instance, if cannabis slows the breakdown of your antibiotic, the drug could build up and increase your risk of side effects like nausea or an upset stomach—issues that already bother about 1 in 10 people on antibiotics, according to the NHS.
On the flip side, if cannabis speeds up the process, your antibiotic might be flushed out too fast, making it less effective against the infection. You can get a deeper dive into how cannabis works with the body’s metabolic pathways to understand why this matters for your treatment.
The specific outcome really depends on the type of antibiotic, the cannabinoids you’re using (THC vs. CBD), your dose, and your own unique metabolism. There’s no one-size-fits-all answer here.
At the end of the day, you want to give your antibiotic the best possible shot at working without anything getting in its way.
Here’s a quick-glance table to help simplify how this metabolic tug-of-war could affect you.
Quick Guide to Cannabis-Antibiotic Interactions
| Type of Interaction | How It Works | What This Could Mean for You |
|---|---|---|
| Enzyme Inhibition | Cannabis (especially CBD) occupies the liver enzymes, slowing down the antibiotic’s breakdown. | The antibiotic stays in your system longer and at higher concentrations, increasing the risk of side effects. |
| Enzyme Induction | In some cases, cannabis can speed up enzyme activity, causing the antibiotic to be cleared out faster. | The antibiotic may not reach or maintain the levels needed to effectively fight the infection, potentially leading to treatment failure. |
| Additive Effects | Both cannabis and some antibiotics can cause similar side effects, like dizziness or an upset stomach. | Using them together could make these side effects feel more intense or uncomfortable. |
Ultimately, understanding these potential interactions is about empowering you to have a more informed conversation with your doctor, ensuring your treatment is both safe and effective.
How Your Liver Processes Cannabis and Antibiotics
To really grasp why mixing cannabis and antibiotics can be tricky, let’s look under the hood at your liver’s role. Think of your liver as your body’s main purification plant, staffed by a highly specialized crew of enzymes known as the Cytochrome P450 (CYP450) system.
Imagine this system is a multi-lane highway, responsible for breaking down and clearing out everything you consume. Here’s the problem: both cannabis compounds (like THC and CBD) and many common antibiotics need to travel in the exact same lanes on this highway.
When you introduce them at the same time, you create a metabolic traffic jam. This isn’t just a theory; it’s a core concept in pharmacology. This backup can play out in two very different ways, each with its own set of risks for your health.
Enzyme Inhibition: The Slowdown Effect
The most frequent interaction is called enzyme inhibition. This is where one substance—in this case, often cannabis, especially CBD—essentially puts up a roadblock on that metabolic highway. It monopolizes the enzymes, slowing down their ability to process anything else.
So, what happens to your antibiotic? It gets stuck in traffic. A practical example: if your antibiotic normally takes 6 hours to be half-cleared from your system, enzyme inhibition could stretch that to 9 or 10 hours. Since it can’t be broken down on schedule, its concentration in your bloodstream climbs higher than intended, seriously ramping up your risk of side effects.
This competition for the same metabolic pathway is the heart of the matter. It also shatters one of the most persistent myths that cannabis doesn’t interfere with other medicines. For a deeper dive into common misconceptions, it’s worth debunking common cannabis myths.
Enzyme Induction: The Speed-Up Effect
Though less common, the opposite scenario can also happen. This is known as enzyme induction. Here, cannabis acts like an overeager traffic cop, signaling the liver to produce more enzymes and push everything through the highway faster.
The result? Your antibiotic gets broken down and flushed from your body way too quickly. It never gets the chance to build up to the therapeutic levels needed to kill the bacteria causing your infection. This can lead to treatment failure, meaning the infection could stick around or get worse, possibly forcing you onto a stronger round of antibiotics later.
Which Antibiotics Have the Highest Interaction Risk?
Not all antibiotics react with cannabis in the same way. The real issue comes down to which metabolic “highway” they use in your liver. Think of it like this: your liver has several lanes, known as CYP450 enzymes, to break down substances.
When an antibiotic and cannabis need to use the same lane, things get congested. This traffic jam is what leads to a potential interaction. Knowing which medications are most likely to cause this bottleneck is the first step in having an informed conversation with your doctor.
Macrolides: The High-Risk Competitors
If one class of antibiotics stands out for its interaction risk, it’s the macrolides. This group includes widely prescribed drugs like erythromycin and clarithromycin.
These antibiotics are powerful inhibitors of the CYP3A4 enzyme—one of the main pathways your body uses to metabolize both THC and CBD. Taking a macrolide essentially puts a roadblock in this lane. If you then introduce cannabis, you create a major pile-up.
This slowdown means that both the antibiotic and the cannabinoids can build up in your system to higher-than-expected levels. The result? You might feel stronger side effects from your medication, like nausea, or the effects of the cannabis could feel much more intense than you’re used to.
Other Antibiotics to Watch
While macrolides are a primary concern, they aren’t the only ones. A few other types of antibiotics also share these metabolic pathways and can create a moderate risk.
- Fluoroquinolones: Drugs like ciprofloxacin are also handled by CYP450 enzymes and can interfere with how your body clears other substances.
- Antifungals: Certain antifungal medications, such as ketoconazole, are sometimes used to treat bacterial infections. They are potent enzyme inhibitors and can cause similar slowdowns.
- Clindamycin: This specific antibiotic has been flagged in pharmacological research for its potential interaction, underscoring the need for caution.
The crucial takeaway is that the interaction depends entirely on the specific drug. An antibiotic from a different class, like amoxicillin, may use different metabolic pathways and pose a much lower risk of a significant interaction.
To help you see where your prescription might fall, the table below breaks down the risk levels for common antibiotic classes. It’s a great way to quickly see if your medication is one that warrants a more detailed chat with your doctor.
Common Antibiotics and Their Potential Interaction Risk with Cannabis
The following table organizes common antibiotics by their primary metabolic pathway and highlights their potential for interacting with cannabis.
| Antibiotic Class | Example Drugs | Shared CYP450 Pathway | Potential Interaction Risk |
|---|---|---|---|
| Macrolides | Erythromycin, Clarithromycin | CYP3A4 (Strong Inhibitors) | High: Significant potential to increase levels of both the antibiotic and cannabinoids, raising the risk of side effects. |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | CYP1A2, CYP3A4 | Moderate: Can slow the metabolism of cannabis, potentially leading to stronger or prolonged effects. |
| Tetracyclines | Doxycycline, Minocycline | Various, including CYP3A4 | Low to Moderate: Some potential for interaction, but generally considered less risky than macrolides. |
| Penicillins | Amoxicillin, Penicillin V | Primarily renal (kidney) excretion | Low: These antibiotics are not heavily metabolized by the liver’s CYP450 system, so the risk of a metabolic traffic jam is minimal. |
| Cephalosporins | Cephalexin (Keflex) | Primarily renal (kidney) excretion | Low: Similar to penicillins, these are less likely to compete with cannabis for liver enzymes. |
Remember, this table is a starting point, not a substitute for professional medical advice. Your own health, the dosage you’re taking, and how often you use cannabis all factor in. The most reliable guidance will always come from a pharmacist or your doctor, who can give you advice tailored to your specific situation.
Turns Out, Cannabis Has Its Own Antibacterial Punch
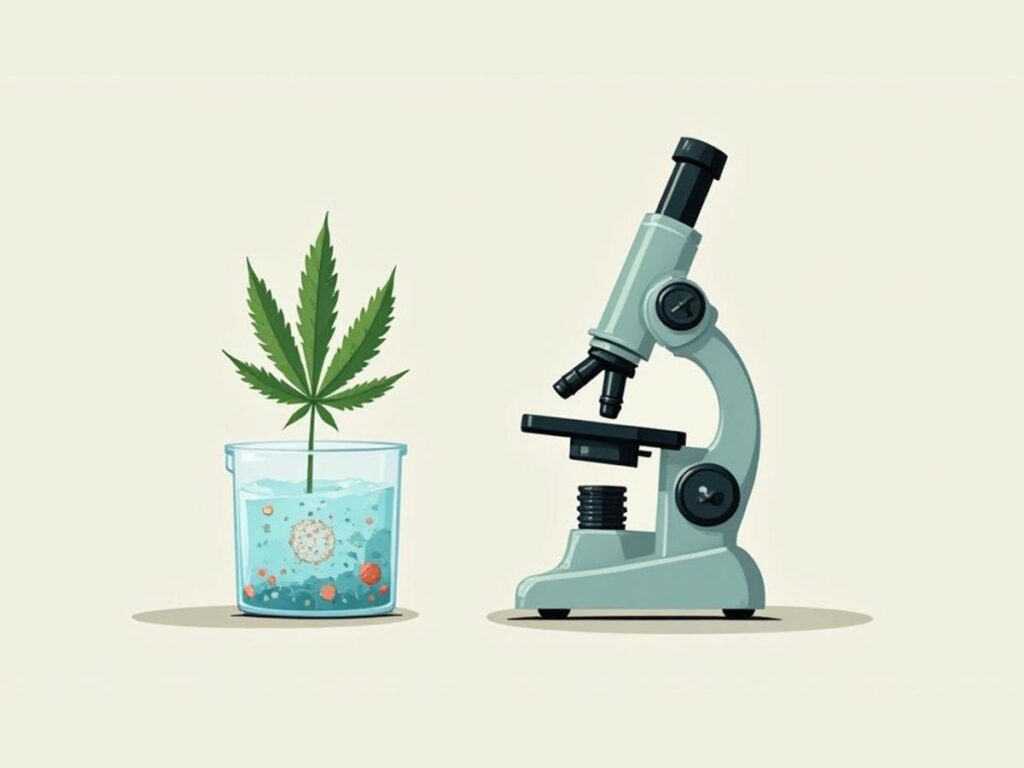
So far, we’ve focused on the potential risks of mixing cannabis and antibiotics. But there’s another side to this story, and it’s a fascinating one. It turns out, the cannabis plant itself might be a powerful ally in the fight against infections.
While the research is still young, early findings are turning heads. Scientists are discovering that compounds within cannabis, known as cannabinoids, could one day be used to take down some of the most stubborn, drug-resistant bacteria we face. This shifts the conversation from a simple interaction to something much more complex and promising.
A New Weapon Against Nasty Bugs
Most of the excitement centers around cannabidiol (CBD), the well-known, non-intoxicating compound in cannabis. Since it doesn’t cause a “high” like THC, it’s a prime candidate for medical research. People are already looking into its potential for a wide range of issues, from anxiety to migraine relief with CBD.
But when it comes to infections, CBD has shown some truly remarkable abilities. A major study in 2020 found that CBD was highly effective at killing a wide variety of Gram-positive bacteria. These are the culprits behind many serious illnesses.
The study showed CBD could take down serious threats like Staphylococcus aureus (the bug behind staph infections and MRSA) and Streptococcus pneumoniae (a leading cause of pneumonia). This is a big deal, suggesting cannabis-derived compounds could fight infections in a completely new way.
What really makes this exciting is the growing threat of antibiotic resistance, which the World Health Organization calls one of the biggest threats to global health. Because cannabinoids like CBD attack bacteria differently than our current antibiotics, they could be a game-changer.
How CBD Fights Back
This isn’t just about killing bacteria in a lab dish. The research dove deeper and found that CBD is exceptionally good at destroying bacterial biofilms. Think of a biofilm as a slimy, protective fortress that bacteria build around themselves. This shield makes them incredibly resistant to antibiotics. By smashing through that shield, CBD could leave the bacteria exposed and vulnerable.
Better yet, research published in Communications Biology showed that bacteria don’t seem to develop resistance to CBD easily. In the study, they saw a major drop in Staphylococcus aureus populations within 48 hours of CBD exposure. This is a huge advantage over traditional antibiotics, which bacteria are getting better at outsmarting every day. You can dig into the specifics by exploring the complete findings of this groundbreaking research.
Now, it’s crucial to put this into perspective:
- This is not a green light to treat an infection with cannabis. We are still in the very early stages of research.
- The doses and preparations used in labs are highly concentrated and can’t be matched by the cannabis products you buy at a dispensary.
- The key takeaway is the potential. We’re talking about future drug development, not a DIY remedy you can use today.
This research just goes to show how incredibly complex the cannabis plant is. So, while you absolutely need to be careful about mixing cannabis with your prescribed antibiotics, it’s incredible to think that one day, a solution to dangerous infections might come from this very same plant.
Practical Safety Rules for Cannabis Users

Navigating the world of cannabis and antibiotics doesn’t have to be complicated. Once you understand the potential for interaction, the game plan becomes simple: play it safe. Your goal is to let your antibiotic do its job effectively without creating unnecessary risks.
This isn’t about judgment; it’s a practical playbook for making the smartest choices while you get better. These straightforward rules will help protect your health and set you up for a much more productive conversation with your doctor.
Rule 1: Be Radically Honest with Your Healthcare Team
This is the golden rule. Your doctor and pharmacist aren’t there to judge you for using cannabis; their job is to keep you safe. Hiding your consumption habits ties their hands and stops them from providing the best care.
They need the complete picture to assess the real risk of a drug interaction. When you talk to them, be specific:
- What you use: Is it THC-heavy flower, a CBD oil, or balanced edibles? Different cannabinoids impact your body’s metabolism differently.
- How much you use: A daily user has a different risk profile than an occasional user. If you microdose 5mg of an edible daily, that’s useful information.
- How you consume it: Smoking, vaping, and edibles all change how your body processes cannabinoids. Let them know your go-to method.
Total transparency gives your healthcare team the information they need to make smart calls, like choosing an antibiotic with a lower interaction risk or advising a temporary break from cannabis.
Rule 2: Become Your Own Health Detective
While on antibiotics, your body is already working overtime to fight an infection. Adding cannabis to the mix means you need to be extra tuned in to how you’re feeling. Pay close attention to any new or worsening side effects, as this could be a sign of an interaction.
Keep a mental—or even a written—log. For instance, your antibiotic might be known to cause mild nausea. But if you feel overwhelmingly sick right after using cannabis, that’s a red flag.
Key Takeaway: Don’t just brush off new or stronger side effects as “normal.” Symptoms like extreme drowsiness, dizziness, a severely upset stomach, or feeling far more intoxicated than usual could mean the drug levels in your body are out of whack. Report these changes to your doctor immediately.
Rule 3: Finish Your Full Antibiotic Course
This is non-negotiable medical advice, and it’s even more critical when other substances are in play. You must finish the entire course of antibiotics your doctor prescribed, even if you start feeling better halfway through.
Stopping early is a dangerous gamble. It allows the hardiest bacteria to survive, multiply, and potentially cause a relapse. If side effects are the issue, call your doctor—don’t just decide to stop on your own.
Rule 4: Discuss Pausing or Reducing Your Cannabis Use
The simplest path forward is often the best. Ask your doctor if it makes sense to pause or reduce your cannabis use while on medication. This is the easiest and safest way to remove any guesswork from the equation.
You might also consider if how you consume matters. Edibles go directly through the liver, creating a bigger “traffic jam” for the enzymes that also process your antibiotic. Smoking or vaping bypasses this initial liver metabolism, but the cannabinoids still end up there eventually. While the diverse range of cannabis products in Sin City offers plenty of choices, none of them completely erase the risk. Your doctor is the best person to help you navigate these details and build a plan that puts your recovery first.
What You Really Need to Know About Cannabis and Antibiotics
Let’s pull it all together. You’re unlikely to see headline warnings about cannabis and antibiotics, but that doesn’t mean the risk is zero. The potential for a significant interaction is real and deserves your attention.
The core of the issue is a metabolic “traffic jam” in your liver. Both cannabis compounds and many antibiotics are broken down by the same enzymes. When taken together, they compete for these enzymes, which can throw off how your antibiotic is processed.
This bottleneck can go one of two ways. It might cause the antibiotic levels in your blood to spike, increasing the risk of side effects. Or, it could cause your body to clear the drug too quickly, making it less effective at fighting your infection.
Your Most Important Next Step
We’ve walked through how this competition in your liver works, identified the riskiest antibiotics, and even explored the antibacterial properties of cannabis itself. But if you remember only one thing, make it this: your health is not a one-size-fits-all situation.
The only way to guarantee your safety and ensure your treatment works is to talk openly with your doctor or pharmacist. They are your absolute best source for advice tailored to you.
Your personal health history, the exact antibiotic you’re taking, and your cannabis habits all come into play. A healthcare professional is the only one who can weigh these factors and give you the right guidance.
They might suggest switching to an antibiotic that doesn’t compete on the same metabolic pathways, or they may simply recommend you pause cannabis use until the infection is cleared.
Ultimately, this is all about being proactive. Being honest with your medical team gives them the information they need to protect you and help you get better. When it comes to your health, don’t guess—get professional medical advice.
Frequently Asked Questions
You’ve got the basics, but a few specific questions are probably still on your mind. Let’s tackle some of the most common ones to give you complete clarity.
Is It Safer to Use CBD Instead of THC with Antibiotics?
This is a common misconception. It’s easy to assume that because CBD isn’t intoxicating, it must be the safer option to mix with medications. When it comes to antibiotics, that’s not the case.
The real issue is the metabolic competition in your liver, where both CBD and THC vie for the same CYP450 enzyme pathways that break down medications. Some research suggests CBD can be an even stronger inhibitor of these enzymes than THC. This means CBD could be more likely to slow your body’s processing of an antibiotic, potentially increasing drug levels and the risk of side effects.
The takeaway? CBD is not a safe alternative to THC when you’re on antibiotics. It poses a similar, and in some cases greater, risk of interaction. Treat CBD with the same caution as THC when discussing medications with your doctor.
How Long Should I Wait Between Doses?
It sounds logical, right? Just wait a few hours between taking your antibiotic and using cannabis. Unfortunately, this strategy doesn’t work because the issue isn’t a brief collision but a prolonged traffic jam in your metabolism.
Both cannabinoids and many antibiotics linger in your system for hours, sometimes even days (this is known as their “half-life”). THC, for example, is stored in fat cells and can be active in your system long after the initial effects have worn off.
Because of this, even if you wait several hours, both substances are still present and competing for those same liver enzymes. Spacing out your doses simply doesn’t solve the underlying problem.
Does Smoking Cannabis Avoid the Liver Interaction?
Another great question. It’s true that the route of consumption changes things, but not enough to eliminate the risk.
When you inhale cannabis, cannabinoids are absorbed directly into your bloodstream through your lungs. This bypasses the first, intensive round of liver metabolism (called “first-pass metabolism”), which is why the effects are so rapid.
But here’s the catch: once those cannabinoids are in your blood, they still have to be broken down and cleared out. And that process happens in the liver. So, while they take a different route, they still end up at the liver, competing with your antibiotic for those crucial CYP450 enzymes. The risk is still there, whether you smoke, vape, or use edibles.
At Wallflower Cannabis House, our team is always ready to help you understand our products. We can’t give medical advice, but we can definitely guide you through our premium selection. You can check out everything we have to offer online at Our Cannabis Store.